One of the widely raised questions is “How is AI Changing Healthcare for Doctors and Should They Be Concerned”? AI is no longer knocking on the door of medicine, it is already in the room. From clinical documentation to diagnostics, artificial intelligence is altering how healthcare is developed, evaluated, and refined. But what does the reality of AI change for those doctors on the ground who are facing overflowing OPDs, complex cases, and challenging patients that require more than just efficiency to manage?
The issue is not just what AI can do, it is what it will mean for doctors. Is this a smarter collaboration? Or the gradual depletion of human hands? Let’s look beyond the hype to the reality.
When AI Helps the Healer: Relief From Administrative Exhaustion
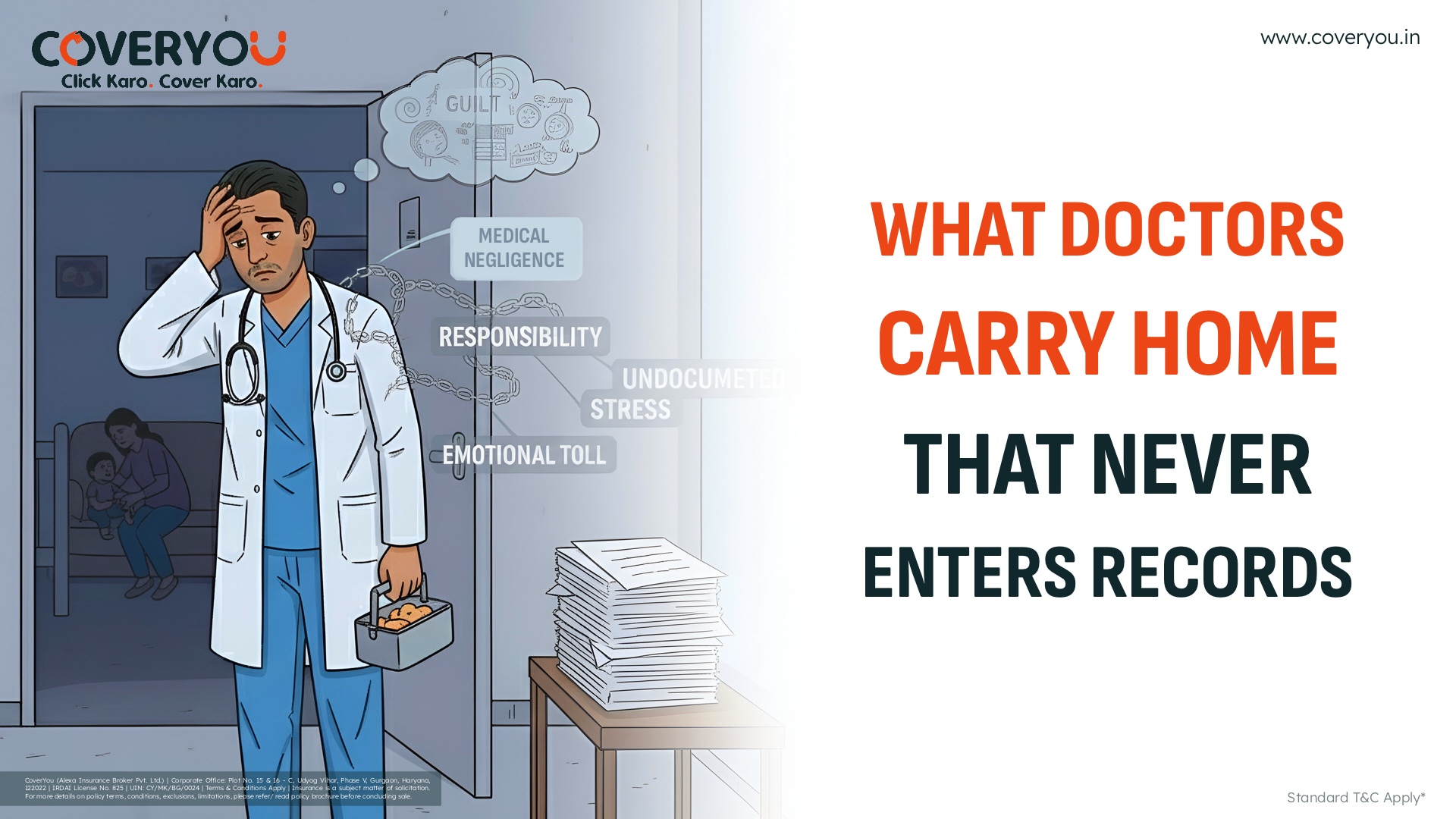
If you have ever spent your evenings after work catching up on patient notes instead of catching up on family time, you are not alone. The administrative burden has been one of the largest contributors to doctors’ burnout. In this case, AI is not just a tool, it is a lifeline.
Ambient AI scribes are one example. These tools are now capturing clinical conversations in real-time and drafting summaries for EMR, giving doctors back their hours and their evenings. A recent 2025 JAMA Network Open study showed it was possible to reduce the amount of time spent taking notes by 20.4% and the amount of time each doctor spent on after-hours charting by 30% when using AI tools. At the University of Iowa Health Care, burnout rates before AI-supported documentation were 32.5% and decreased to below 25% once doctors began using AI-supported documentation. This is not in the future. It has already been a life-changing resource!
From Clinical Chaos to Clarity: AI as a Thought Partner
Artificial intelligence can find data patterns that would take a human hours or days to find. AI doesn’t take away medical judgment, it optimizes it. At Intermountain Health, AI algorithms support clinician’s ability to detect early behavioral health risks. At Parkland Hospital, the suicide prevention model identifies high risk patients prior to the presentation of traditional symptoms.
These tools do not diagnose for you, they help you better diagnose. As Yale researchers stated, the right AI does not replace doctors, it allows doctors to return to what matters: less paperwork, more presence; less screen time, more time at the bedside.
A Growing Threat: Collaboration Meets Efficiency
Of course, not everything about the slow march toward AI is refreshing. Many within specialties like radiology and pathology have a latent fear of machines moving from augmenting clinical reasoning to unteachable substitution. A Stanford study in 2024 showed that GPT-4 achieved a 92% diagnostic accuracy with real patient cases. At UCLA, the SLIViT model used 3D-image episode recall and deep learning to describe an individual patient’s risk of disease faster than clinical working groups could.
The worry is hardly science fiction anymore. The real question is, when AI is cheaper, faster, and often better than MDs at clinical reasoning, what will stop institutions from utilizing machines instead of MDs? This is not paranoia. It is a warning.
The Concealed Bias Underneath the Code
Bias in medicine has been troublesome. But now it’s not only human, it’s algorithmic. AI systems learn from data. If the data is biased, incomplete, or historically biased, the outputs will be as well. Misdiagnosis, delayed interventions, or biased recommendations can all happen.
And trust? It’s fragile. Only 12% of baby boomers trust AI will their care. Younger patients are still hesitant. Doctors are placed in the middle and must trust tools they didn’t develop, explain decisions they didn’t solely make, and justify outcomes that have been dictated by a black box.
Your Data May Be Smarter, But It Is Also in Danger
Behind every smart AI tool is a massive pool of patient data. And the data? It is under attack. Cyberattacks on healthcare have skyrocketed. AI models can distort the diagnosis or provide erroneous treatment if they are manipulated. And although the data was anonymized, it’s becoming easier and easier to re-identify using technology.
When a breach happens, it isn’t the developers or vendors that will talk to families that are in crisis. It is going to be the doctor who used the system, trusted it and thought it was safe.
So What’s The Doctor’s Role Going to Look Like in the Age of AI?
At the end of the day, and after stripping away all terminology and headlines, the doctor’s role hasn’t changed at a basic level; heal, listen, hold. It may suggest a diagnosis, but it doesn’t experience the hesitation in the patient’s voice. This may chart faster, but it doesn’t comfort the mother waiting for results. It may recognize patterns, but it did not take a moment, sit in silence, and know what that silence meant. As AI continues to reshape healthcare, it is our role to ensure that we do it with doctors, not around doctors.
Conclusion: AI Can Help. You Can Only Care
The history of medicine is a dance between emerging tools and human truths. AI is now the latest partner in that dance. It can help us think smarter, see better, and act faster. The machine cannot replicate the heartbeat of empathy. The instinct built over the ears. The trust earned over the years in a single consultation. So use AI. Become proficient at it. But don’t lose sight of why you got into medicine. Let the machines calculate. Let the doctors care.